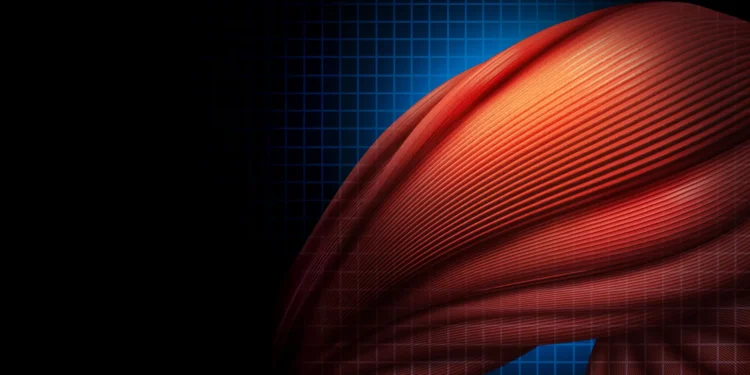
At the cellular scale, the way muscle tissue repairs itself becomes surprisingly complex. The body does not respond the same way to all forms of damage. A sudden muscle tear from a sports injury differs greatly from the slow decline in muscle strength seen in conditions such as muscular dystrophy.
A research team at Cincinnati Children’s has uncovered a shared and unexpected repair process that may help the body recover from several kinds of muscle damage. The findings were published online on Nov. 21, 2025, in Current Biology. The project was led by first author Gyanesh Tripathi, PhD, and corresponding author Michael Jankowski, PhD, who oversees the Research Division in Cincinnati Children’s Department of Anesthesia and serves as Associate Director of Basic Science Research for the Pediatric Pain Research Center.
The newly identified mechanism involves macrophages, a type of immune cell. These cells are usually known for acting like tiny cleanup crews that remove bacteria, dead cells, and other unwanted material.
A Neuron-Like Repair Signal
“The biggest surprise about this was finding that a macrophage has a synaptic-like property that delivers an ion to a muscle fiber to facilitate its repair after an injury,” Jankowski says. “It’s literally like the way a neuron works, and it’s working in an extremely fast synaptic-like fashion to regulate repair.”
Scientists have long known that macrophages respond to muscle injury by releasing cytokines and chemokines that create inflammation, influence pain, and help drive the growth and regeneration of muscle fibers.
Searching for Pain Relief Leads to a Different Breakthrough
The research team originally aimed to uncover ways to ease pain during recovery after surgery. They were looking for clues that could eventually reduce the need for pain medications that carry significant side effects.
Although they did not find a new approach for pain relief, they identified a process that makes muscle repair occur more quickly. This discovery may support the development of future treatments for muscle wasting and acute injuries. The findings also suggest that macrophages might eventually serve as specialized “delivery vehicles” for cell-based therapies targeting a wider range of medical conditions.
“These are infiltrating macrophages, a very specific type. They’re not ones already residing in the tissue. These come in after damage occurs,” Jankowski says.
Real-Time Evidence of Rapid Muscle Activation
In experiments that used mouse models of two different injury types, researchers examined how macrophages interact with the myofibers that form muscle tissue. They were even able to capture key moments of this activity as it occurred.
By using brief bursts of a designer chemical to activate the macrophages, the team observed these immune cells forming synaptic-like contacts with myofibers. The macrophages then released calcium ions directly to the muscle fibers, accelerating early stages of healing. Within 10 to 30 seconds, the researchers measured bursts of electrical activity inside the damaged muscle.
“This occurs in a very rapid fashion. You can activate the macrophage and make the muscle twitch subtly almost immediately,” Jankowski says.
Healing Effects Seen in Both Injury and Disease Models
The same type of macrophage-driven signaling also helped mice with disease-like muscle damage. After recognizing the injury, the immune cells gathered at the site and triggered waves of activity in the muscle fibers. After 10 days, mice that received this treatment had substantially more new muscle fibers than mice in the control group.
“A similar synaptic-like response worked in both scenarios,” Jankowski says.
Next Research Steps
More work is needed to determine whether human macrophages behave the same way when muscle is injured. If they do, researchers will still need to learn how to guide or control the process in ways that could be safely used as therapy.
The team is also interested in an unexpected outcome: although the infiltrating macrophages sped up healing, they did not appear to reduce acute pain. Understanding why this occurs may help explain why about 20% of children who undergo surgery continue to experience lingering pain afterward.
Looking ahead, the researchers want to explore whether macrophages can deliver other helpful signals or materials to muscle cells.
Cincinnati Children’s co-authors include Adam Dourson, PhD, Fabian Montecino-Morales, PhD, Jennifer Wayland, MS, Sahana Khanna, Megan Hofmann, Hima Bindu Durumutla, MS, Thirupugal Govindarajan, PhD, Luis Queme, MD, PhD, and Douglas Millay, PhD. The Bioanalysis and Imaging Facility at Cincinnati Children’s also contributed to the work.
Funding for this research came from grants provided by the National Institutes of Health (R01NS105715, R01NS113965, R61/R33AR078060, R01AR068286, R01AG082697) and the Cincinnati Children’s Hospital Research Foundation.